Welcome to RCNC's Recovery Blog!
If you want to be in the know about what’s going on at our organization, you’ve come to the right place.
Be sure to subscribe to our monthly e-newsletter here.
We are thrilled to announce that the 12th Annual Capital Rally for Recovery will take place on September 28, 2024, from 11:00 AM to 2:00 PM at Mordecai Historical Park in Raleigh, NC. This event has become a cornerstone in our community's efforts to raise awareness about recovery and to celebrate the strength and resilience of those who have overcome substance use disorders.
In the heart of Raleigh, a transformative event is set to take place on February 23rd at the RCNC Creative Corner Fashion Show. This unique showcase not only celebrates the beauty of fashion but also sheds light on the therapeutic benefits of expressive arts. The theme, "Recovery to Discovery," captures the essence of this creative journey that promises to be an evening filled with inspiration, resilience, and self-discovery.
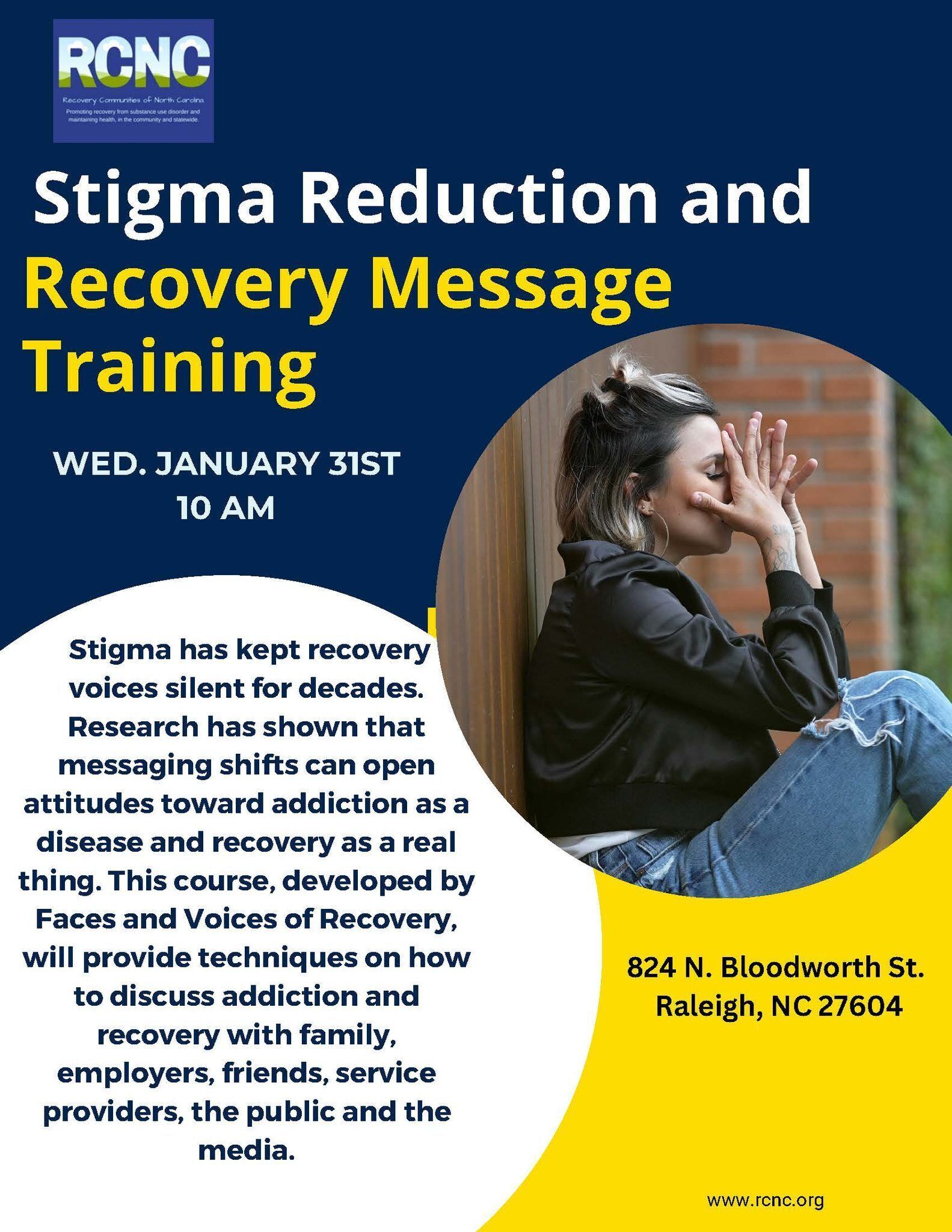
Stigma has long been the silent adversary of those on the recovery journey. For decades, individuals battling addiction have faced a world mired in misconceptions and judgments, preventing their voices from being heard and their stories from being shared. Recognizing the need for a transformative change in public perception, the Recovery Communities of North Carolina (RCNC) has organized a groundbreaking Stigma Reduction and Recovery Message Training scheduled for January 31st at 10:00 AM.
Join us for a fantastic evening at the Chavis Memorial Park Community Center in Raleigh, NC. Admission is only $5.
Put on your dancing shoes and come celebrate the holiday season with us. Let's create lasting memories together. See you there! Click on the read more button to view more details.
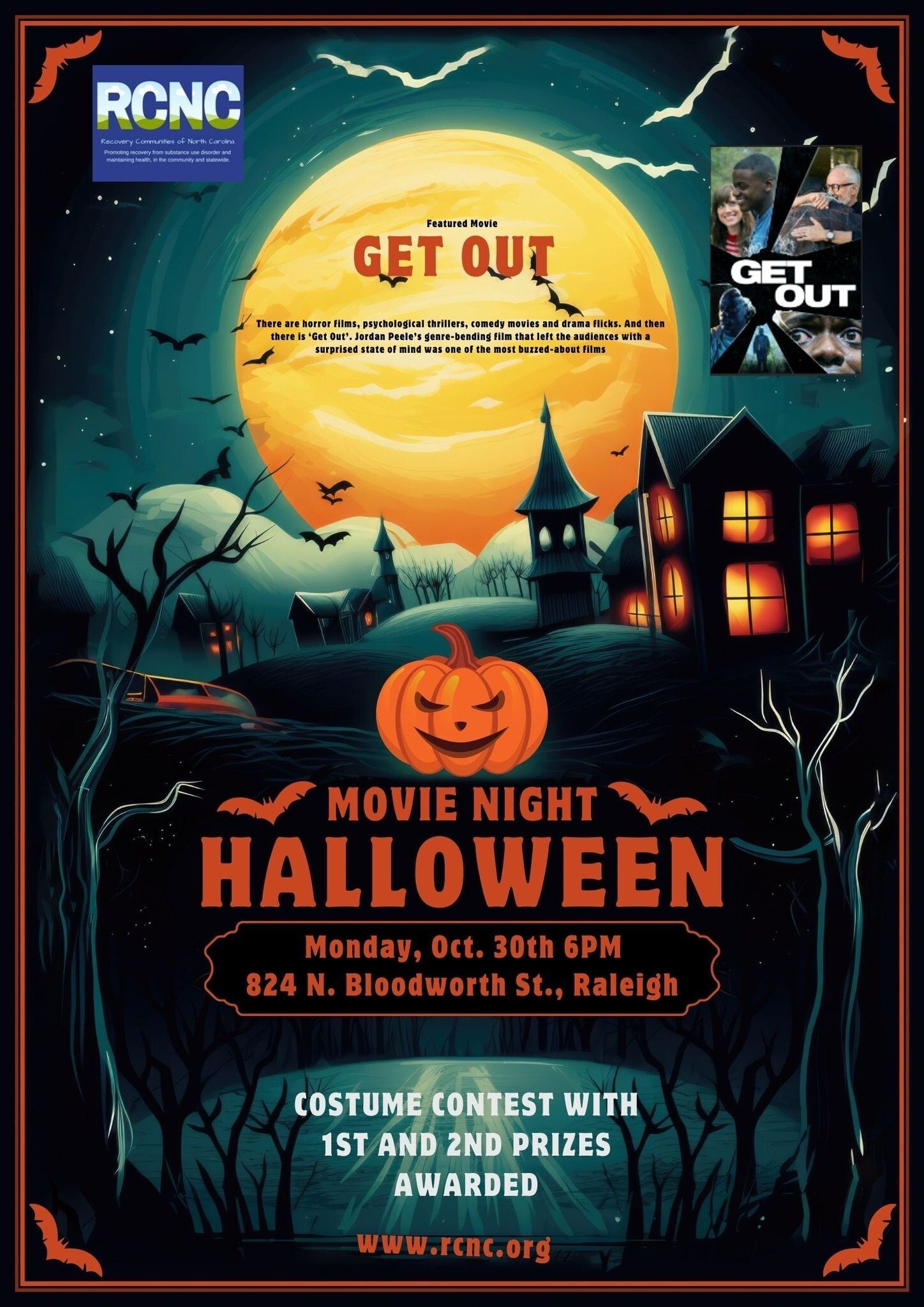
You're invited to join us for a Halloween-themed movie night filled with chills, thrills, and unforgettable fun as we celebrate recovery in style! Date: Monday Time: 6:00 PM. We'll be screening the hair-raising and thought-provoking movie "Get Out" to set the perfect Halloween mood. Buckle up for an eerie and exhilarating journey! Costume Contest: Show off your most creative Halloween costumes inspired by the movie, and you could win fantastic prizes! There are awards for the top two spooktacular outfits. This is your opportunity to connect, share your recovery stories, and strengthen the bonds that make recovery a journey filled with hope and support.
Recovery is a journey of transformation and rediscovery, an opportunity to reclaim your life and build a future that's in harmony with your true self. At the heart of this transformative journey lies the practice of self-care, an essential and personalized approach to fostering wellness. #RecoverySupport and self-care are not one-size-fits-all; rather, they're tailored to fit your needs, preferences, and unique path to recovery. As we celebrate #RecoveryMonth, let's delve into the realm of self-care and explore how it can be a guiding light on this road to redemption.